Surgery for Congenital Defects of the Hand


Carpel tunnel syndrome can cause tingling, numbness, or a dull ache in the shaded area shown in this illustration.

The surgeon makes an incision from the palm to the wrist, providing access to the tissue that’s causing pressure on the nerve.

A section of tissue is cut, relieving pressure on the nerve and restoring feeling and function to the hand.

In Dupuytren’s contracture, scar-like tissue in the palm pulls fingers into an abnormal position. The surgeon may make zig-zag incisions across this band of tissue, creating small skin flaps.
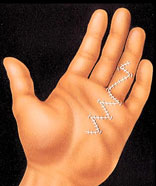
After surgery the repositioned flaps expand like an accordion, allowing freer finger motion.

In a typical syndactyly, two fingers are fused together. The surgeon often uses zig-zag incisions to separate the fingers, creating triangular skin flaps.

Skin flaps cover most of the exposed areas between the fingers. Skin grafts are used to fill the shaded areas at the base of the fingers.
Hand Surgery and Your Plastic Surgeon
Dramatic advances have been made in recent years in treating patients with hand injuries, degenerative disorders, and birth defects of the hand. At the forefront of these advances have been plastic surgeons-specialists whose major interest is improving both function and appearance. Plastic surgeons undergo intensive training in hand surgery, and they (along with orthopedic surgeons and general surgeons) treat patients with a wide range of hand problems.
This information is designed to give you a basic understanding of the most common hand problems-what they are, what plastic surgeons can do for them, and the results you can expect. It can’t answer all of your questions, since each problem is unique and a great deal depends on your individual circumstances. Please be sure to ask your doctor if there is anything about the procedure you don’t understand.
If You’re Considering Hand Surgery
If you’re considering hand surgery, a consultation with a plastic surgeon is a good place to start. The surgeon will examine you, discuss the possible methods of treatment for your problem, and let you know if surgery is warranted. If it is, the surgeon will discuss the procedure in detail, including where the surgery will be performed (in the surgeon’s office, an outpatient surgery center, or a hospital), the anesthesia and surgical techniques that will be used, possible risks and complications, the recovery and rehabilitation period, and the probable outcome in terms of function and appearance.
Don’t hesitate to ask your surgeon any questions you may have during the initial consultation-including any concerns you have about the recommended treatment and the costs involved. (Since hand surgery is performed primarily to correct physical abnormalities, it usually is covered by insurance. Check your policy or call your carrier to be sure.)
All Surgery Carries Some Uncertainty and Risk
Thousands of successful hand operations are performed each year. While the procedures are generally safe when performed by a qualified and experienced plastic surgeon, complications can arise.
In all types of hand surgery, the possible complications include infection, poor healing, loss of feeling or motion, blood clots, and adverse reactions to the anesthesia. These complications are infrequent, however, and they can generally be treated. You can reduce your risks by choosing a qualified surgeon and by closely following his or her advice.
Hand Injuries
The most common procedures in hand surgery are those done to repair injured hands, including injuries to the tendons, nerves, blood vessels, and joints; fractured bones; and burns, cuts, and other injuries to the skin. Modern techniques have greatly improved the surgeon’s ability to restore function and appearance, even in severe injuries.
Among the techniques now used by plastic surgeons:
- Grafting – the transfer of skin, bone, nerves, or other tissue from a healthy part of the body to repair the injured part;
- Flap surgery – moving the skin along with its underlying fat, blood vessels, and muscle from a healthy part of the body to the injured site;
- Replantation or transplantation – restoring accidentally amputated fingers or hands using microsurgery, an extremely precise and delicate surgery performed under magnification. Some injuries may require several operations over an extended period of time.
In many cases, surgery can restore a significant degree of feeling and function to injured hands. However, recovery may take months, and a period of hand therapy will most often be needed (see Recovery and rehabilitation below.)
Carpal Tunnel Syndrome
The carpal tunnel is a passageway through the wrist carrying tendons and one of the hand’s major nerves. Pressure may build up within the tunnel because of disease (such as rheumatoid arthritis), injury, fluid retention during pregnancy, overuse, or repetitive motions. The resulting pressure on the nerve within the tunnel causes a tingling sensation in the hand, often accompanied by numbness, aching, and impaired hand function. This is known as carpal tunnel syndrome.
In some cases, splinting of the hand and anti-inflammatory medications will relieve the problem. If this doesn’t work, however, surgery may be required.
In the operation, the surgeon makes an incision from the middle of the palm to the wrist. He or she will then cut the tissue that’s pressing on the nerve, in order to release the pressure. A large dressing and splint are used after surgery to restrict motion and promote healing. The scar will gradually fade and become barely visible.
The results of the surgery will depend in part on how long the condition has existed and how much damage has been done to the nerve. For that reason, it’s a good idea to see a doctor early if you think you may have carpal tunnel syndrome.
Rheumatoid Arthritis
Rheumatoid arthritis, an inflammation of the joints, is a disabling disease that can affect the appearance and the function of the hands and other parts of the body. It often deforms finger joints and forces the fingers into a bent position that hampers movement.
Disabilities caused by rheumatoid arthritis can often be managed without surgery-for example, by wearing special splints or using physical therapy to strengthen weakened areas. For some patients, however, surgery offers the best solution. Whether or not to have surgery is a decision you should make in consultation with your surgeon and your rheumatologist.
Surgeons can repair or reconstruct almost any area of the hand or wrist by removing tissue from inflamed joints, repositioning tendons, or implanting artificial joints. While your hand may not regain its full use, you can generally expect a significant improvement in function and appearance. Still, it’s important to remember that surgical repair doesn’t eliminate the underlying disease. Rheumatoid arthritis can continue to cause damage to your hand, sometimes requiring further surgery, and you’ll still need to see your rheumatologist for continuing care.
Dupuytren’s Contracture
Dupuytren’s contracture is a disorder of the skin and underlying tissue on the palm side of the hand. Thick, scar-like tissue forms under the skin of the palm and may extend into the fingers, pulling them toward the palm and restricting motion. The condition usually develops in mid-life and has no known cause (though it has a tendency to run in families).
Surgery is the only treatment for Dupuytren’s contracture. The surgeon will cut and separate the bands of thickened tissue, freeing the tendons and allowing better finger movement. The operation must be done very precisely, since the nerves that supply the hand and fingers are often tightly bound up in the abnormal tissue. In some cases, skin grafts are also needed to replace tightened and puckered skin.
The results of the surgery will depend on the severity of the condition. You can usually expect significant improvement in function, particularly after physical therapy (see Recovery and rehabilitation.), and a thin, fairly inconspicuous scar.
Congenital Deformities
Congenital deformities of the hand-that is, deformities a child is born with-can interfere with proper hand growth and cause significant problems in the use of the hand. Fortunately, with modern surgical techniques most defects can be corrected at a very early age-in some cases during infancy, in others at two or three years-allowing normal development and functioning of the hand.
One of the most common congenital defects is syndactyly, in which two or more fingers are fused together. Surgical correction involves cutting the tissue that connects the fingers, then grafting skin from another part of the body. (The procedure is more complicated if bones are also fused.) Surgery can usually provide a full range of motion and a fairly normal appearance, although the color of the grafted skin may be slightly different from the rest of the hand.
Other common congenital defects include short, missing, or deformed fingers, immobile tendons, and abnormal nerves or blood vessels. In most cases, these defects can be treated surgically and significant improvement can be expected.
Recovery and Rehabilitation
Since the hand is a very sensitive part of the body, you may have mild to severe pain following surgery. Your surgeon can prescribe injections or oral medication to make you more comfortable. How long your hand must remain immobilized and how quickly you resume your normal activities depends on the type and extent of surgery and on how fast you heal.
To enhance your recovery and give you the fullest possible use of your hand, your surgeon may recommend a course of rehabilitation (physical and occupational therapy) under the direction of a trained hand therapist. Your therapy may include hand exercises, heat and massage therapy, electrical nerve stimulation, splinting, traction, and special wrappings to control swelling. Keep in mind that surgery is just the foundation for recovery. It’s crucial that you follow the therapist’s instructions and complete the entire course of therapy if you want to regain the maximum use of your hand.

